Safe, easy to obtain and spontaneous, stem cells help rats recover from a stroke
Transplanting stem cells that can migrate to and spontaneously repair damaged tissue improves stroke recovery in rats, according to research conducted at Tohoku University1 . These stem cells, called multilineage-differentiating stress-enduring (Muse) cells, overcome drawbacks of other stem cell types, and are thus promising for treating stroke in humans.
Mari Dezawa, who led the work with Teiji Tominaga at Tohoku University, said that the perfect stem cell for use in humans is one that effectively regenerates tissue but does not cause tumors, is readily accessible and is easy to administer. "We demonstrate that Muse cells satisfy these demands," says Dezawa.
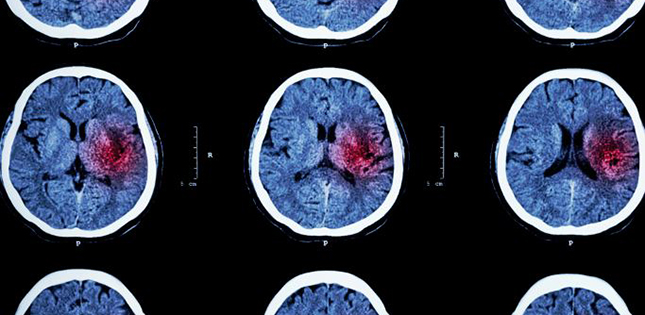
The predominant cause of stroke is blockage of a blood vessel in the brain by a blood clot. The obstruction damages cells in the oxygen-starved area (called the infarct). Stem cells have the potential to replace some of the damaged cells and restore brain function, but many types of stem cells are difficult to obtain for practical or ethical reasons, some have limited benefits, while others carry a high risk of tumors. To test whether Muse cells offer a better solution, Dezawa and Tominaga mimicked stroke in rats by blocking the middle cerebral artery to starve their brains of oxygen.
Before injecting Muse cells into the rats, the researchers had to obtain them from adult human skin and develop them into neurons in culture. Whereas most other types of stem cells must be 'induced' to develop into a specific cell type prior to transplantation via the introduction of specific genes, the neuronal development of Muse cells is spontaneous.
The researchers then injected the Muse cells into the damaged region of the rats' brains. While the transplanted cells did not reduce the infarct size, treated animals performed better than untreated animals on neurological tests within 12 weeks. Furthermore, many of the transplanted cells survived for at least 84 days and integrated into the rat brains as functional neurons that reconstructed complex neural circuits, but did not cause tumors.
The scientists say that the safety and efficiency of Muse cells mean that they offer a new strategy for treating stroke, which could soon be tested in humans. "Our technique could be used to treat acute to subacute stroke," says Tominaga. "We now need to prepare for transplantation of Muse cells in humans by selecting the source of cells, and then developing the manufacturing process. We expect this to take two to three years."
- Reference:
1. Uchida, H. et al. Transplantation of unique subpopulation of fibroblasts, Muse cells, ameliorates experimental stroke possibly via robust neuronal differentiation. Stem Cells advance online publication, 28 September 2015.
DOI: 10.1002/stem.2206
Contact:
Mari DezawaGraduate School of Medicine
mdezawa@med.tohoku.ac.jp